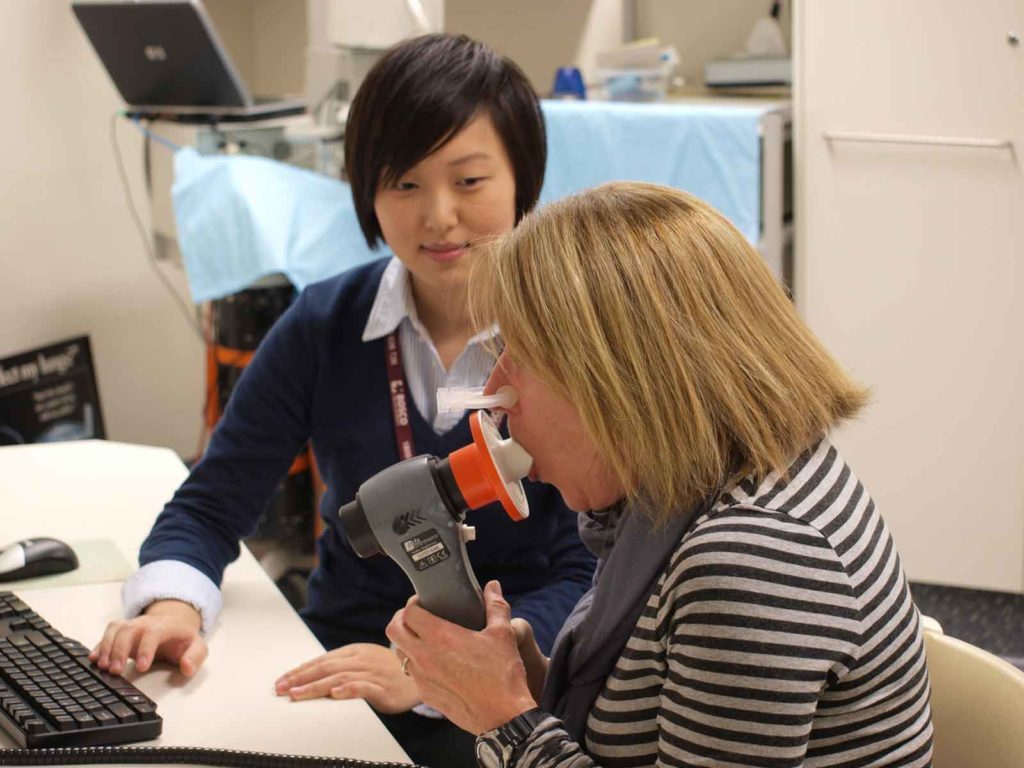
There are a range of lung function test that you may undergo to help you treating health professional understand exactly what is going on with your respiratory help. Different tests will help to understand more about how you lungs are functioning and if you may have an obstructive lung disease, like COPD, or a restrictive lung disease, such as Pulmonary Fibrosis. Watch the video to hear more from respiratory scientist Iain Smith or read on below.
Where do I get a lung function tests?
Getting a lung function test can be performed at multiple different areas. You can get them performed at a GP’s practice, specialist clinics or at hospital-based clinics. Under the current COVID recommendations it may be a little bit tricky to get, or some GPs may not be offering it. If that’s the case then they may be able to refer you on to a specialised respiratory clinic.
What disease or conditions can be diagnosed with lung function tests?
Iain says lung function tests, or respiratory function tests, doesn’t necessarily diagnosis a condition. They help with the diagnosis, but your diagnosis will also take into account other factors involving your signs and symptoms and medical history. A lung function test, like spirometry, gas diffusion, and some long volume measurements, cab assist in identifying if you have an obstructive lung disease like COPD or asthma or bronchiectasis. Or if you have a restrictive lung disease which is more of the interstitial lung disease, like asbestosis or Pulmonary Fibrosis. Occasionally some people will have a mixed pattern which is a combination – for example, asthma and Pulmonary Fibrosis.
What is the difference between a peak flow meter reading and spirometry?
Iain explains that peak flow meter is a lung function test that measures the peak speed, or velocity, that you can exhale, but it provides you with very little other data. It can be quite useful for individuals with asthma or COPD, as a peak flow meter can often identify if you’re having a flare up of your condition, but however that’s it’s limitation. Spirometry on the other hand provides a lot more information. It tells us the peak flow, as well as how much air you can breathe in and blow out and how much air you can blow out in that first second.
With a peak flow meter you don’t get the same information, so you won’t be able to diagnose or assist with the diagnosis of, say, COPD because it doesn’t provide enough information. So, if COPD is what the GP is potentially looking at or potentially believes you may have spirometry will help them understand that.
What is bronchial provocation testing?
Iain says you may be referred for a bronchial provocation test is if the doctor believes that you may have asthma and you’ve had other investigations and they haven’t found a diagnosis. During bronchial prevocational testing you will receive an inhaled substance and to try cause a reaction in the airways similar to that of an asthma attack. You will get increasing doses to see if you experience a change in your forced exhaled volume in the first seconds of an exhale and if there is a change in that over the increasing doses that you’re given.
I’m worried about getting a bronchial provocation test, what can I do?

If you’re feeling apprehensive before the bronchial provocation test, remember it’s performed in a safe environment with trained professionals there to assist. You’re inhaling very small doses. When we start to see signs that your airways are potentially getting a little bit tighter, then once you’ve hit 15% of your baseline level, we stop the test, provide you with a bronchodilator (which can we Ventolin or Asmol) and then we measure to make sure you return back to your normal levels.
What is a FeNO test?
FeNO, or ‘fractionally exhaled nitric oxide’ is a lung function test which assesses the airway inflammation of the lungs. Dependent if you have a condition like asthma for example, your airways may produce a certain chemical marker and that releases nitric oxide. During the test you will need to blow out for about 8-10 seconds at a medium speed. During this the inflammation when you blow out is measured. This is usually performed on individuals that have asthma, or in some cases COPD. It’s helps your treating team understand how responsive your airways could be to certain types of medication. For example, if you have an elevated FeNO score, you may be more suited for a certain type of inhaler.
What is a DLCO/gas infusion test?
DLCO, otherwise known as a gas diffusion test, looks at how well the lungs actually absorb oxygen. It’s a test performed primarily at a respiratory clinic or a hospital and it’s similar to spirometry. It involves you holding your breath for around 8-10 seconds before blowing back out again. During that breath hold time, you’re inhaling a test gas which is primarily room air – so it’s nitrogen and oxygen – with two tracer chemicals. One is carbon monoxide and the other one is primarily methane. The carbon monoxide is used to measure how the gases are absorbed into the body. The methane itself doesn’t get absorbed in the body but the carbon monoxide absorbs quicker than oxygen. When you take that deep breath and you’re holding your breath for 8 seconds before blowing out, it’s giving your body a chance to absorb the carbon monoxide and when blow back out we can measure what’s happened. This test assists with the diagnosis of COPD and Pulmonary Fibrosis. What it will do is assess the severity of any impairment in the actual diffusion of the gas.
What is a Body Plethysmography?
Body plethysmography measures your lung volume by measuring how much air is in them after you take a deep breath and how much is left after you exhale. It’s performed while you’re sitting in a booth to control the volume of air. The test helps to identify any abnormalities of the overall lung size. You will likely perform a handful of panting manoeuvres – very shallow breathing like a suck and blow or push/pull against a shutter for a few seconds. You will then perform a long blow out followed by a deep breath in and a long blow back out again. Some people may find this test a little bit confronting because you are inside a closed booth. Remember you can let yourself out easily at any time. The respiratory specialist or the allied health taking you through the test will be able to assist you with that if you’re having any difficulties.
How can I understand the results of my lung function test?

If you’ve had a respiratory function test and you’re uncertain of what’s happened or want to know more information about it, ask your referring health professional how you did on the test and to explain the results. They may say that, for example, your airways are obstructed but what effect does that actually mean? Ask your treating health professional about the outcome of the tests and they will be able to explain it to you.

Connect to care
Our Our highly skilled nurse can provide guidance on all aspects of your condition according to the management guidelines. The free Respiratory Care Nurse service is telephone-based and available for people living with COPD or bronchiectasis. Free call 1800 654 301 or complete the form via the link below.
Was this page helpful?
Good job! Please give your positive feedback
How could we improve this post? Please Help us.



